Hallux rigidus
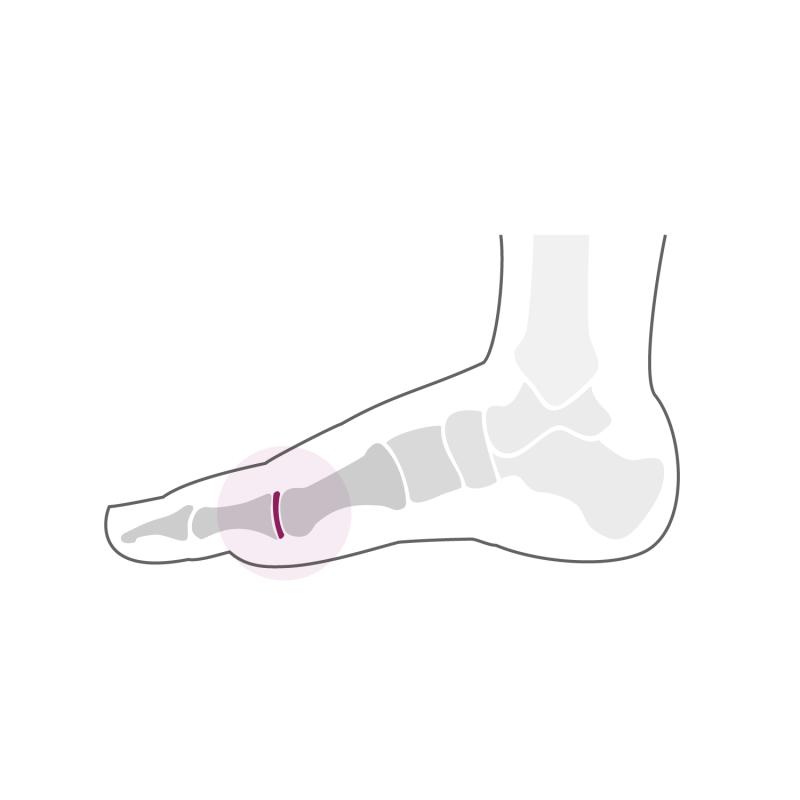
Hallux rigidus ("rigidus" means rigid in Latin) refers to the osteoarthritis of the big toe’s joint. This osteoarthritis (wear of the articular cartilage) is manifested by a decrease in joint mobility and by pain in the region of the joint and discomfort when wearing closed shoes. The main cause of this osteoarthritis is "primary", that is to say that it occurs without any particular trauma. Even if we do not know the exact mechanism that leads to the degradation of articular cartilage, we often observe the development of this arthritis in relation to a rather flat morphology of the head of the 1st metatarsus. In this particular shape of the head of the 1st metatarsus, the stresses suffered by the cartilage are higher on the internal and external edges of the articular surface, mainly when the big toe is subjected to rotational movements. This leads to "asymmetrical" wear of the cartilage and joint incongruence. Once the articular surfaces of the 1st metatarsus and 1st phalanx of the big toe no longer "pass" together, the wear of the cartilage will only progress over the years. Osteoarthritis can also develop following direct trauma to the joint of the big toe, especially following intra-articular fractures with direct damage to the cartilage.
The increased pressure on the bone due to the decrease in the thickness of the cartilage will cause the production of bone, so-called osteophytes or bone spurs. These bone spurs will irritate the joint capsule that surrounds the joint and cause mechanical irritation of this structure and the first pain. There are therefore two types of pain in osteoarthritis of the big toe joint, pain due to pressure from osteophytes on the joint capsule and joint pain from osteoarthritis due to contact with bone surfaces exposed to cartilage. This arthritis will only slowly get worse over time causing more or less significant symptoms.
Treatment
Initially, the treatment is conservative and consists of adapting the shoe with the aim of avoiding pressure on the back of the foot. One can also use plantar supports provided with a carbon zone under the joint of the big toe aimed at decreasing the range of motion, a kind of "resting" of the joint. In this phase we often associate a local anti-inflammatory treatment (application of ice or anti-inflammatory gel), physiotherapy for anti-inflammatory purpose and an adaptation of daily burdens (limitation of walking or other restrictive activities on the foot).
If the pain and discomfort persist despite this conservative treatment, surgical solutions can be proposed. In case of sufficient conservation of articular cartilage in the central area of the joint and capsular irritation due to osteophytes, a "joint cleaning" aimed at resecting osteophytes can be very effective and helps maintain some joint mobility . Often, however, this intervention, which can be performed on an outpatient basis, will certainly delay the progression of osteoarthritis but will not be able to completely stop it. If the osteoarthritis is too large and the cartilage of the load zone is reached and the symptoms become more and more disabling, arthrodesis (blockage) of the joint of the big toe in neutral position remains the first solution choice. If the surrounding joints are intact at the time of the arthrodesis, this blockage of the joint of the big toe is very well tolerated and allows again to perform restrictive activities on the foot such as hiking, sports "stop-and -go "and even running. In rare cases, if the cartilage of the plantar area of the head of the 1st metatarsus is still intact, a rotational osteotomy of the head of the 1st metatarsus may be offered in order to move the articular cartilage from the plantar area to the central area of load and thereby maintain joint mobility.
Joint reconstruction requires wearing a shoe with a rigid sole for a period of two weeks after the intervention. The wearing of conventional shoes is possible from the 3rd week. The foot remains tender and swollen up to 8-10 weeks post-operatively. In the case of a rotational osteotomy or arthrodesis, wearing a rigid sole shoe is done for 6 weeks. A radiological check at 6 weeks post-operative confirms bone consolidation. Physiotherapy in the form of lymphatic drainage and gait rehabilitation is then undertaken in order to improve the function of the foot. Activities such as swimming or cycling are possible from the 7th week after the operation. More restrictive activities such as hiking or running are possible from the 4th month. The function of the foot improves up to 1 year post-operatively, when clinical and radiological monitoring is carried out at the end of treatment.
In order to be complete, we should mention the possibility of replacing the articular surface of the joint of the big toe with a prosthetic implant. There are several types of prostheses available. However, the results published in the literature are in our view unsatisfactory and correspond to the experience encountered during our consultation. After the placement of such an implant, the joint most often remains painful, joint mobility remains reduced and these implants have a strong tendency to loosen, especially in active patients. The revision of such a loosened implant is a complicated surgery requiring in the majority of cases the placement of a bone graft taken from the iliac crest and causing painful convalescence with most often a disappointing final functional result. Given these findings and as the results of the long-term arthrodesis are very encouraging, we do not offer prosthetic replacement for osteoarthritis of the big toe joint.
