Ankle Arthritis
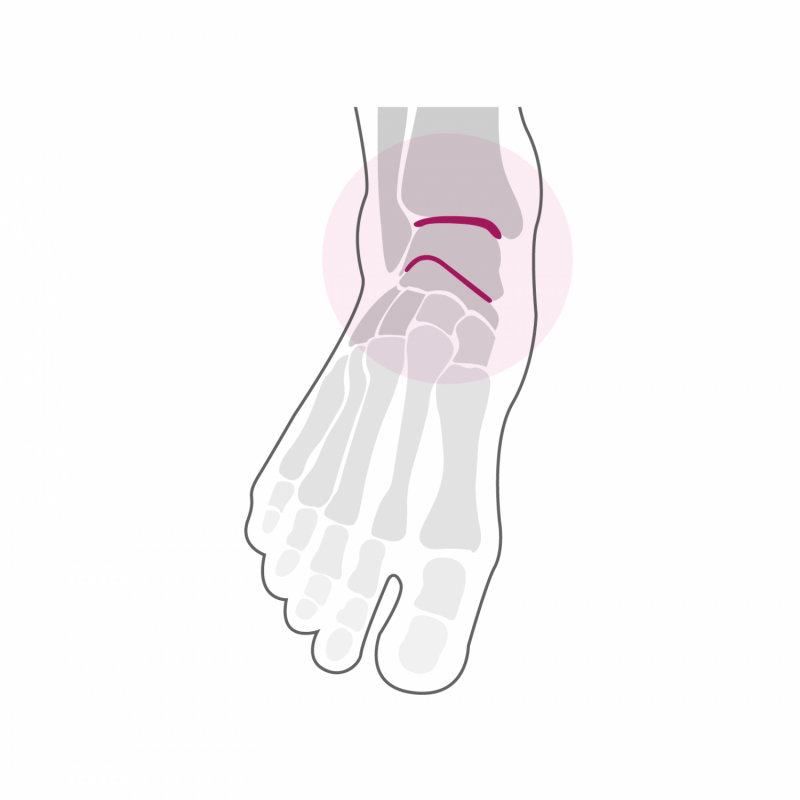
Like osteoarthritis of the midfoot or hindfoot, osteoarthritis of the ankle can be primary - with no apparent cause - or secondary, most often following a fracture that affected the joint surface. In the case of post-traumatic osteoarthritis, symptoms can appear several years after the initial trauma, but can also occur much faster, after a few months already. Other diseases such as hemophilia (repeated bleeding in the joints due to a lack of clotting factor) or hemochromatosis (too high red blood cell count) can cause severe osteoarthritis of the ankle.
In addition to the pains felt firstly on exertion and at rest, as well as in the morning upon waking up or or after a long sitting position, osteoarthritis of the ankle manifests itself in most cases also by a marked decrease in joint mobility. The diagnosis is confirmed by clinical examination and a radiological assessment.
Treatment
Conservative treatment is done by local anti-inflammatory measures and possibly oral anti-inflammatory drugs. Adjusting loads by reducing certain pain-causing activities and putting on appropriate footwear can relieve symptoms. Intra-articular infiltration of hyaluronic acid and / or cortisone may also be effective temporarily. However, osteoarthritis tends to progress over time.
If conservative measures no longer provide sufficient pain relief, surgical treatment should be considered. If the osteoarthritis is not yet too advanced on the radiological level and concerns only part of the joint, an operation aimed at maintaining joint mobility while slightly modifying the axis of the hindfoot allows improve symptoms, such as; a corrective osteotomy which can be performed above the ankle (supra-malleolar osteotomy) or below the ankle (infra-malleolar osteotomy performed at the calcaneus). These measures make it possible to slow down the progression of osteoarthritis, but their indications are limited to well-selected cases.
As the ankle joint is essential for the overall mobility of the foot, arthrodesis of this joint should be avoided if possible. The arthrodesis remains a valid option in the treatment of advanced osteoarthritis of the ankle, but the loss of mobility of the ankle can have harmful consequences on other joints of the foot as well as other joints of the leg, such as; the knee or hip. If the anatomical conditions and the quality of the bone allow it, we currently prefer in most cases the total ankle replacement. Replacing the joint helps maintain joint mobility and is very effective against pain due to osteoarthritis. The new generation total ankle prostheses benefit from more than 30 years of observation and offer completely satisfactory results. However, this is a technically difficult procedure that must be performed by a specialist experienced in foot surgery. The total ankle prosthesis, like that of the knee or the hip, has a limited lifespan which currently amounts to 12 to 15 years (data from the specialized literature). In most cases, the prosthesis will begin to loosen over time, which can cause pain. In case of sufficient bone quality, a change of prosthesis using a so-called revision prosthesis is possible, which still allows joint mobility to be maintained and thus spares the neighboring joints. If a replacement of the prosthesis is no longer possible due to insufficient bone quality or the development of a joint infection, arthrodesis can still be performed, however requiring the placement of a bone graft removed at the level of the iliac crest (pelvic bone).
During arthrodesis, the cartilage remaining on the articular surfaces is completely eliminated and the two bones are prepared in such a way that they can be fixed together in order to obtain a bony "bridge" at the joint. The arthrodesis is stabilized using screws or plates, most often made of titanium, material which does not necessarily have to be removed later.
When a total prosthesis is put in place, the articular surfaces are completely replaced by the prosthetic components. The cuts in the bone are made in a personalized way on the basis of a pre-operative planning on scanner, which guarantees an optimal and anatomical position of the implants. The intervention can last up to two hours depending on any associated gestures and can be performed under general or spinal anesthesia. It can be combined with local anesthesia of one of the main nerves of the foot (popliteal block), which significantly reduces post-operative pain. It takes two to three nights of hospitalization. Walking is done immediately from the first post-operative day in full discharge of the foot operated using canes in a removable plastered boot. This total discharge must be observed during the first two weeks. The removal of stitches and the making of a new removable plastered boot take place 2 weeks after the intervention. From this moment, a partial load of 15 to 20 kg on the operated foot is allowed for 4 additional weeks. A clinical and radiological check-up is carried out 6 weeks after the operation.
In case of sufficient bone integration of the implants, a progressive increase in the load on the ankle is done over a period of two to three weeks until the total load. From the 7th week, a physiotherapy treatment aimed at reducing the swelling of the foot and improving its function is implemented. Resumption of activities such as swimming, cycling or moderate walking is possible from the 10th post-operative week. More restrictive activities on the foot such as longer hikes can be considered from the 7th month after the intervention. Activities such as running or other stop and go sports are not recommended after arthrodesis or the fitting of a total ankle prosthesis. The ankle will continue to refine and heal for up to one year post-operatively and gradually regain its full function. Clinical and radiological checks are then carried out once a year during the first three years, then every two years from the third year after the intervention.
